Our new tool in the war against antibiotic-resistant superbugs: Personalized drug-dosing devices
The way we prescribe antibiotics to patients who need them is broken.
Taking one-size-fits-all, imprecise levels of the drugs increases the risk of toxicity—or treatment failure. At the same time, taking too-low doses of any given antibiotic increases the risk of population antibiotic resistance.
On the one hand, you have a danger for the individual patient. On the other hand, a global public health threat. Either way, with antibiotics still our best tool against microbial infections, these risks are ones we need to take.
Or are they?
Taking a page out of endocrinology’s book, researchers from around the world are studying the use of therapeutic drug monitoring (TDM) and precision dosing for antibiotics using skin patches connected to wearable devices.
Welcome to precision antibiotics.
How would precision dosing for antibiotics work?
For critically ill hospitalized patients, the stakes of failing treatment or experiencing drug toxicity are especially high.
At the same time, the pharmacokinetics in play can be more complicated than in a healthy patient. Intensive care patients receive extra fluids, which may dilute drug concentrations. And vacillating blood pressure means drugs are being cleared by the kidneys at changing rates.
That’s why getting dosing just right is so important—and challenging—in these contexts. Hence, hospitals’ worldwide increasingly turning to TDM for individualized antibiotic dosing for critically ill patients.
The technique, which relies on a chromatography test and dose adjustment based on carefully calibrated results, is most commonly used to monitor the use of vancomycin and aminoglycosides, which have a very narrow therapeutic window. Over the past few years, the technique has also increasingly been used to track levels of beta-lactams.
But TDM is imperfect for truly precise antibiotic dosing. It requires time and access to a chromatography lab. This is possible for some hospitalized patients—but not for all.
That’s where precision dosing comes in.
A team at Imperial College London developed and tested a system for bedside antibiotic precision monitoring. It relies on a patch that tracks levels of phenoxymethylpenicillin in the blood.
Where did the idea come from? The clinical researchers were inspired by the microneedle biosensors used to monitor blood glucose levels for diabetes patients. And to take that inspiration further, the researchers are now working on a system akin to the artificial pancreas: a wearable device to deliver the precise dose of antibiotics per the patch’s measurements.
Another approach from the Netherlands: A research team has developed software called AutoKinetics to help clinicians adjust antibiotic doses using EHR data. The data coming from these trials suggests that this approach to personalized antibiotic dosing is safe and possible.
However, when it comes to the question of improved outcomes, the results are mixed. Accordingly, the team is hoping their next steps—pairing their software with artificial intelligence—will help bring its efficacy to the next level.
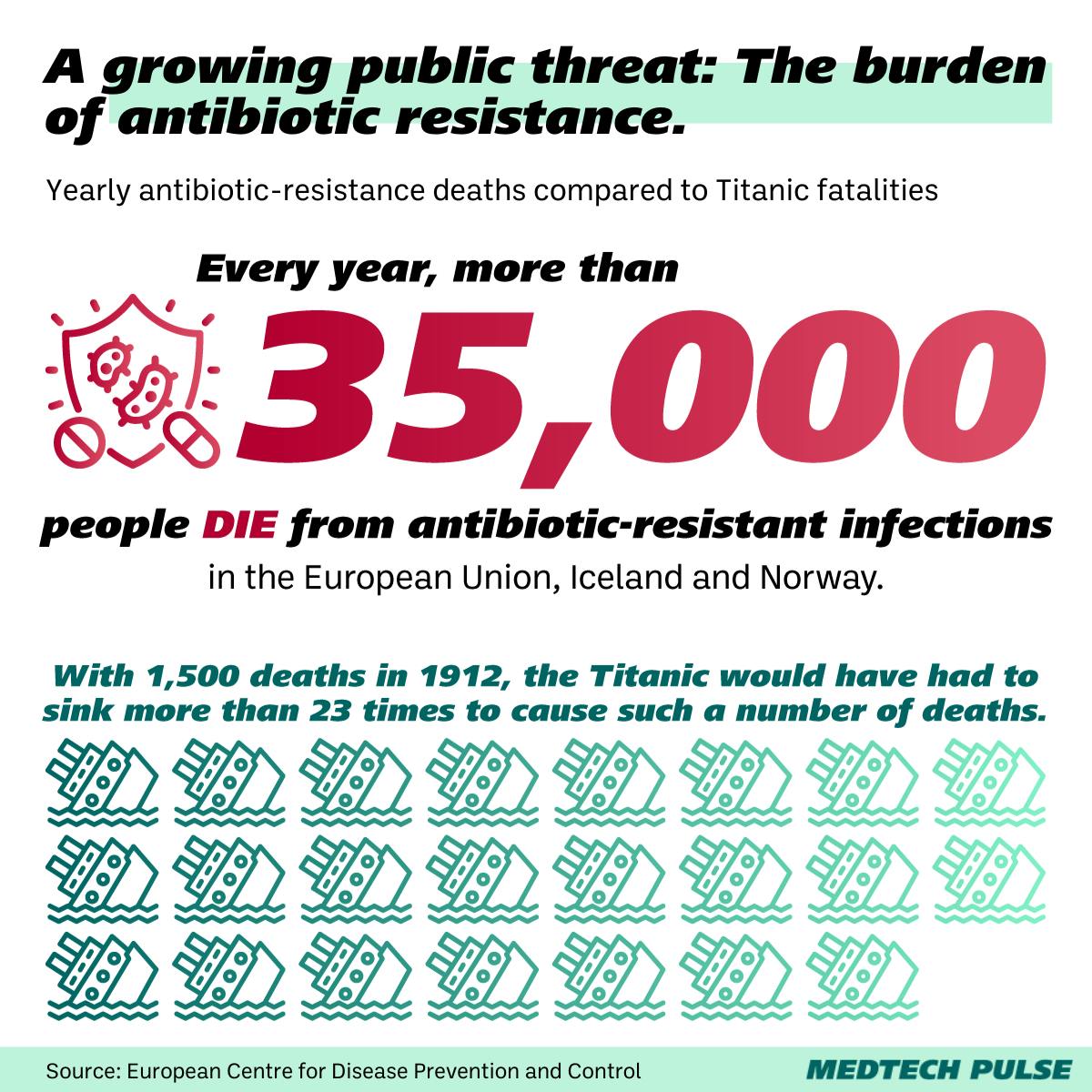
Why this matters: The stakes of antibiotic resistance
As we hinted earlier, we shouldn’t just care about this issue as individuals who may need to take a course of antibiotics once in a while. Say for a throat infection or after surgery.
We must all be invested in this issue because how each person uses antibiotics affects the rest of the world. As more antibiotic-resistant pathogens spread across the world, our food supply, drug design progress, and human life expectancy are all threatened.
To stop this global threat, governments, private entities, and NGOs are working to do their part. Prevention measures include improving infection prevention and control in the first place, improving tracking and diagnostics, developing new vaccines and therapeutics—and yes, continuing to use antibiotics.
Especially given that the majority of antibiotic-resistant infections are linked to healthcare procedures and hospital-acquired infections, hospital-based precision dosing is poised to make a difference.
Researchers continue to make strides in how antibiotic precision dosing improves outcomes. And as we do, we can be grateful for where we’re already seeing a positive difference: Providers are becoming more aware of where and how they may be over- or under-dosing patients. That’s how we’re improving antibiotic stewardship across healthcare—one step at a time.