How EHRs and digital health startups power the food as medicine movement
When you think of medicine, you’re probably not thinking about the sushi you had for dinner. Or the salad you packed for lunch today.
The food as medicine movement will make you rethink that.
Across the U.S., hospitals are seeing improvements across a variety of health indicators for participants in food as medicine programs. These programs can range from grocery budget allowances to hospital-hosted fresh produce “farmacies.”
Here’s where medical technology comes in: EHRs and digital health tools integrating social determinants of health screening are helping these hospitals expand the uptake of food as medicine.
We think these collaborations are an excellent whole-person approach to preventive medicine. Let’s take a closer look at how these program work and what our industry can learn from these successes.
What is food as medicine?
In a time when weight loss drugs—and their ability to keep people from eating—are being touted as the best new thing in healthcare, food as medicine takes the opposite approach.
The movement draws from principles of nutrition, public health, and behavioral health to design preventative interventions using food. In other words, food as medicine positions healthy eating as a way to prevent, manage, and treat illness.
The movement responds to a global crisis. More worldwide deaths are attributable to “suboptimal diet” than to any other health risk factor—including tobacco. In the U.S., despite the country’s wealth, this issue is compounded by the widespread existence of food deserts—which leave millions of Americans hungry and malnourished.
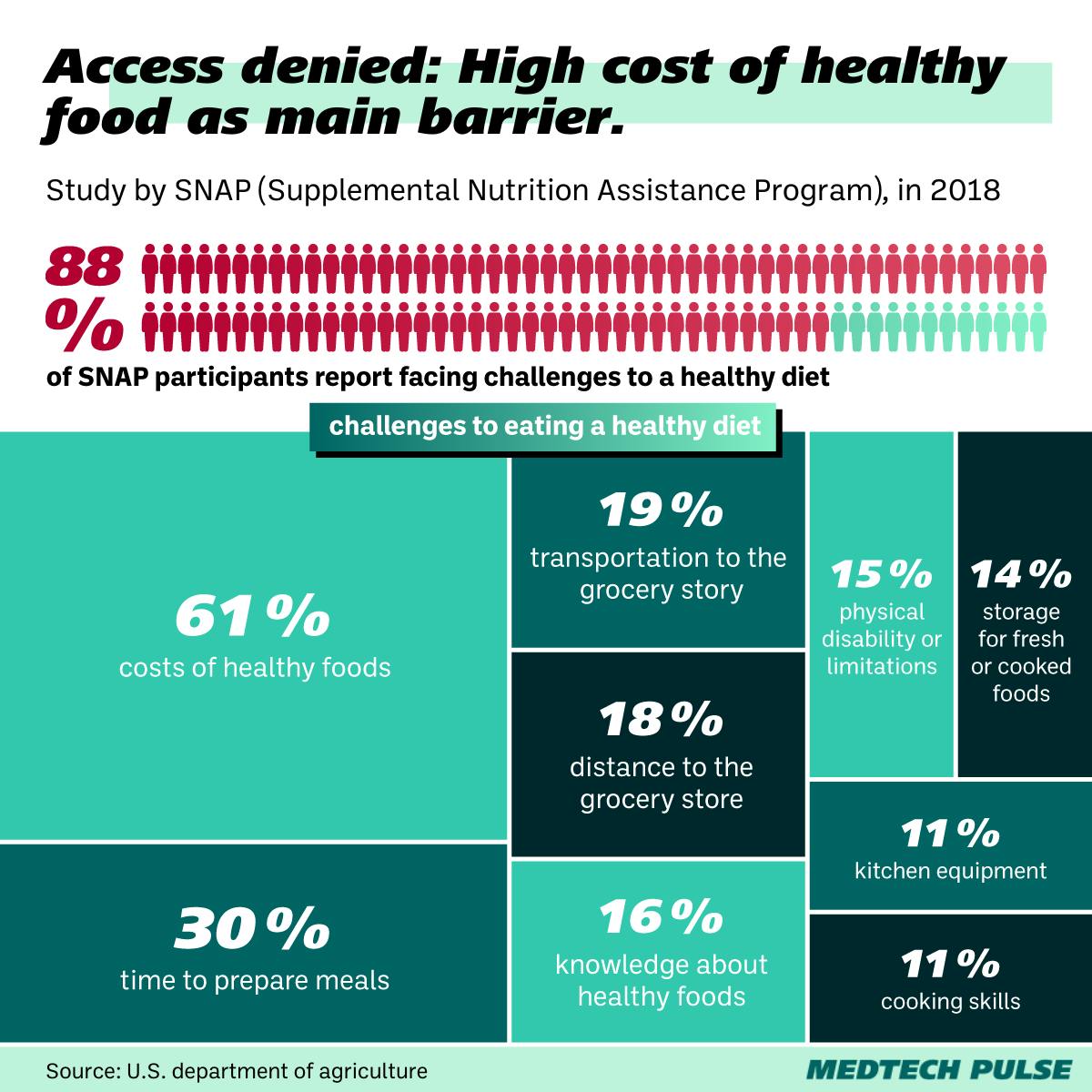
And even when healthy food is available, it’s often unaffordable for the people who need it the most.
Luckily, American hospitals have begun taking notice of this issue, employing food as medicine principles into their patient and community health programs.
In New York City, St. Barnabas Hospital partners with community organization Project EATS to provide patients with food insecurity, diabetes, and hypertension with fresh farm stand food through their onsite food pantry, rooftop garden, greenhouse, and even beehives. In Pennsylvania, Geisinger’s Fresh Food Farmacy has successfully helped patients lower A1C levels, visit the Emergency Department less frequently, and overall engage in more preventive care.
And while nutrition is not a magical panacea for all ailments (if only!), nutrition-based health education empowers patients to take better care of themselves overall.
“Focusing on nutrition may not necessarily take away that chronic disease, but we have seen instances where it’s helping patients to manage their symptoms a little better and hopefully improve their quality of life,” said Catherine Hill, health educator for community outreach and partnerships at Augusta Health, which has been operating its own Food Farmacy for the past five years.
Food as medicine goes digital
What’s fueling these programs’ success? The use of digital tools and EHR integrations to refer eligible participants and help clinicians monitor their progress.
One example of such a tool is startup Neighborly’s social care platform, which can be integrated directly into the Epic EHR. This is how Geisinger’s food as medicine program has seamlessly fit into the rest of the health system’s offerings. Now, everyone on a patient’s care team—from their dietitian to their primary care provider to their pharmacist—can be on the same page about the patient’s nutrition progress.
“By integrating Neighborly and making it launchable within the electronic health record, it now becomes part of the workflow in the clinical enterprise and an important component of the patients’ records,” said Brian Ebersole, senior director of health innovations at Geisinger, who oversees the Fresh Food Farmacy.
Geisinger has also developed its own app for the Fresh Food Farmacy, allowing participants to directly schedule food pick-up, get recipes, connect with care team members, and monitor their progress.
Food as medicine as a model for preventive health innovation
Ultimately, we’re excited about food as medicine (and the digital health tools supporting it) because of how simple and effective an initiative it is.
Whole-person approaches to preventive health like this are evidence-based and largely affordable for many health systems to adopt. And as our industry knows, digital health integration and incentive programs make that adoption even easier.
Whether it’s turning GPS trackers into medical devices for field primary care, offering prescriptions for air conditioning during heat waves, or reframing vegetables as medicine—many of today’s largest public health crises sometimes require creative, but ultimately simple innovations.
With this context in mind, we’ll leave you with this. Sometimes, our job as medtech innovators is to shoot for the moon with our newest technological offerings. Other times, our responsibility is not to design the most complex new technology but to find new digital ways to support grassroots preventive health initiatives. It’s through this balanced approach to innovation that we’ll uncover a healthier future for the whole world.