Behavioral telehealth exploded in the pandemic. Prescription regulation threatens further growth.
A locked bathroom in a family home. A parked car outside a shared apartment.
These are two of the places psychotherapy patients and providers found themselves conducting visits in 2020.
The early days of the COVID-19 pandemic forced many specialties to adapt to a new normal of telehealth — behavioral health was no exception.
In fact, with the months and years ahead, the availability of telehealth visits correlated with an increase in overall behavioral health utilization.
Yet, as we’ve moved past the pandemic’s first year, lawmakers and regulators have had to grapple with how to regulate behavioral telehealth outside of a public health emergency scenario.
Behavioral health utilization went up during the pandemic
It’s not hard to believe that the pandemic has been associated with a significantly increased prevalence of mental illness.
Many people were isolated and less active, people’s safety and economic security were threatened worldwide, there was an increase in morbidity and mortality — all of these factors reasonably contributed to psychological distress.
At the same time, many health systems limited in-person nonemergency care — or even stopped offering it altogether. Telehealth became the stopgap.
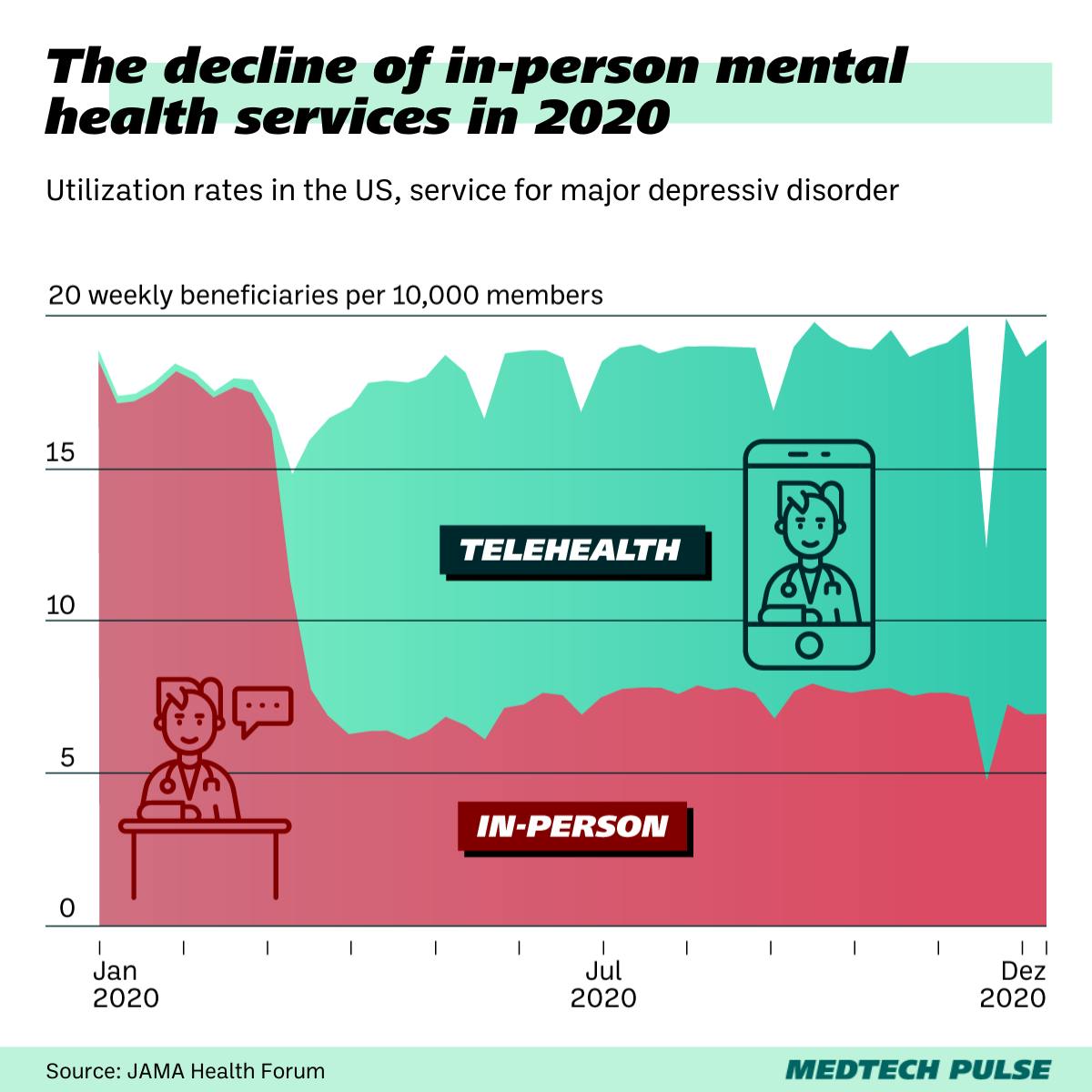
In fact, a study published in JAMA Health Forum earlier this month showed that, while in-person mental health services declined by over 50% after the public health emergency was declared, behavioral telehealth utilization rates increased by a factor of 16–20.
This trend held true across all five of the most common mental health diagnostic categories: major depressive disorder, anxiety disorders, bipolar disorder, adjustment disorder, and posttraumatic stress disorder (PTSD).
The study, which tracked claims for 5 million privately-insured adults in the U.S., reported that mental health services for some conditions even increased by 10–20% from January to December 2020.
Behavioral telehealth will likely remain beyond the public health emergency
Sometime this year, the COVID-19 public health emergency declaration in the U.S. is expected to expire. When that happens, regulations accounting for broader telehealth coverage and access will also expire.
But that doesn’t mean outpatient behavioral care will return to how it used to be. Many patients (and providers) have gotten used to the comfort and accessibility of virtual care — and COVID is likely to remain a threat even when the emergency declaration expires.
Plus, initial analysis as to the utility of telehealth appears to be promising. As we covered in our last edition, a recent study showed that most telehealth visits don’t require additional in-person follow-up care.
Luckily, Congress has enacted a temporary grace period for telehealth coverage — to give regulators more time to analyze next steps and potentially create a pathway for telehealth accommodations and options to stay.
At the moment, telehealth expansion — for behavioral health and beyond — has broad bipartisan support in Congress. The Connect for Health Act, which currently has more than 60 Senate sponsors, has been introduced to codify more telehealth protections.
A roadblock for behavioral telehealth: prescriptions
However, regulatory barriers threaten to limit the efficacy of behavioral telehealth in one arena: medication-assisted telehealth psychiatry.
The public health emergency’s restriction-loosening measures impacted this area of behavioral health as well, particularly in how it loosened restrictions around the prescription of controlled substances.
The results have been mixed.
On the bright side, access to life-changing care — like opioid use disorder care — increased dramatically with behavioral telehealth’s 2020 growth. Kaiser Health News (KHN) reported that addiction care professionals have seen a significant drop in missed appointments.
On the other hand, loosened drug-dispensing requirements have also meant less follow-up to monitor patients’ protocols. It’s also resulted in what KHN called “allegedly sloppy prescription practices” from some startups in the behavioral telehealth space.
In December, the Substance Abuse and Mental Health Services Administration (SAMHSA) proposed a codification of telehealth regulations on opioid treatment programs. However, the Drug Enforcement Administration (DEA)-regulated portion of the sector remains in limbo. Namely, the DEA has yet to determine how individual providers can register to prescribe buprenorphine via telehealth.
On a smaller scale, the issue is complicated by the actions of individual pharmacies, which have started to become more skeptical toward prescriptions sent to them by telehealth providers — especially startups.
For instance, KHN reported that many pharmacies have been refusing to fill Adderall prescriptions from startups amidst the current shortage of the medication.
So, while policymakers and patients may be optimistic — and even enthusiastic — about behavioral telehealth, skepticism appears to be creeping into the healthcare industry. And even into MedTech itself.
Michael Yang, managing partner at VC firm OMERS Venturies, told KHN that, while telehealth has increased the availability of quality care for many, some actors have allegedly exploited the tool: “You had a lot of people who saw an opportunity to do things that were less than scrupulous.” This includes prescribing medications for mental health conditions without monitoring patients.
One way or another, it’s clear behavioral telehealth is here to stay. It fills huge care access gaps and has become a status quo that’ll be hard to undo.
We hope that regulatory agencies and elected representatives will continue acting on their optimism for telehealth and move to enact much-needed permanent legislation governing these life-saving tools. With these rules in place, behavioral telehealth can confidently continue to grow and better serve patients and providers.