A vitals check on patient data matching: The problem with death records
Interoperability.
Around the world, this is a core goal of many health IT operations and innovators.
Why is interoperability so critical?
It’s simple: Without the seamless flow of data between health entities and EHRs, ER docs miss new medications. Conditions ruled out by a physician in one city are brought up again in another city. A pattern of health crises goes unnoticed by a primary care provider.
Patients suffer when records don’t follow them wherever they get healthcare.
Another issue that arises when records don’t accurately track a patient’s entire health journey? They can miss when a patient dies.
Ghosts in the EHR
UCLA Health Professor Neil Wenger is leading a study that’s uncovering just how pervasive this problem is in his own health system. He and the team wrote a JAMA research letter, published this month.
In an examination of around 12,000 seriously ill primary care patients, Wenger and his co-investigators found that roughly 20% of deceased patients in the sample were marked alive in EHRs, but dead in state public health files.
So, why does this matter? Shouldn’t we be more concerned with data on living patients than leftover data on patients we can’t provide care to anymore?
First, Wenger noted that the numbers were shocking because it was unacceptable for a health system to lose track of such seriously ill patients—especially ones who had been repeat patients for years.
“When I found a bunch of them were dead and we didn’t actually know it, that’s when I said we need to describe it,” he said. “This is a cohort where we need to know about everyone who is dead.”
But these numbers are also concerning because they’re a marker of a bigger problem. This study has made headlines because, in the U.S., there’s no nationwide benchmark yet for how frequently mix-ups like these happen. Wenger’s study appears to be the first to offer a quantified estimate.
The patient data matching conundrum
The prevalence of deceased patients in EHR systems points to how well—or how poorly—patient record matching is going.
Of course, this prevalence is likely to vary across different health systems, depending on the stringency of state and regional data regulations.
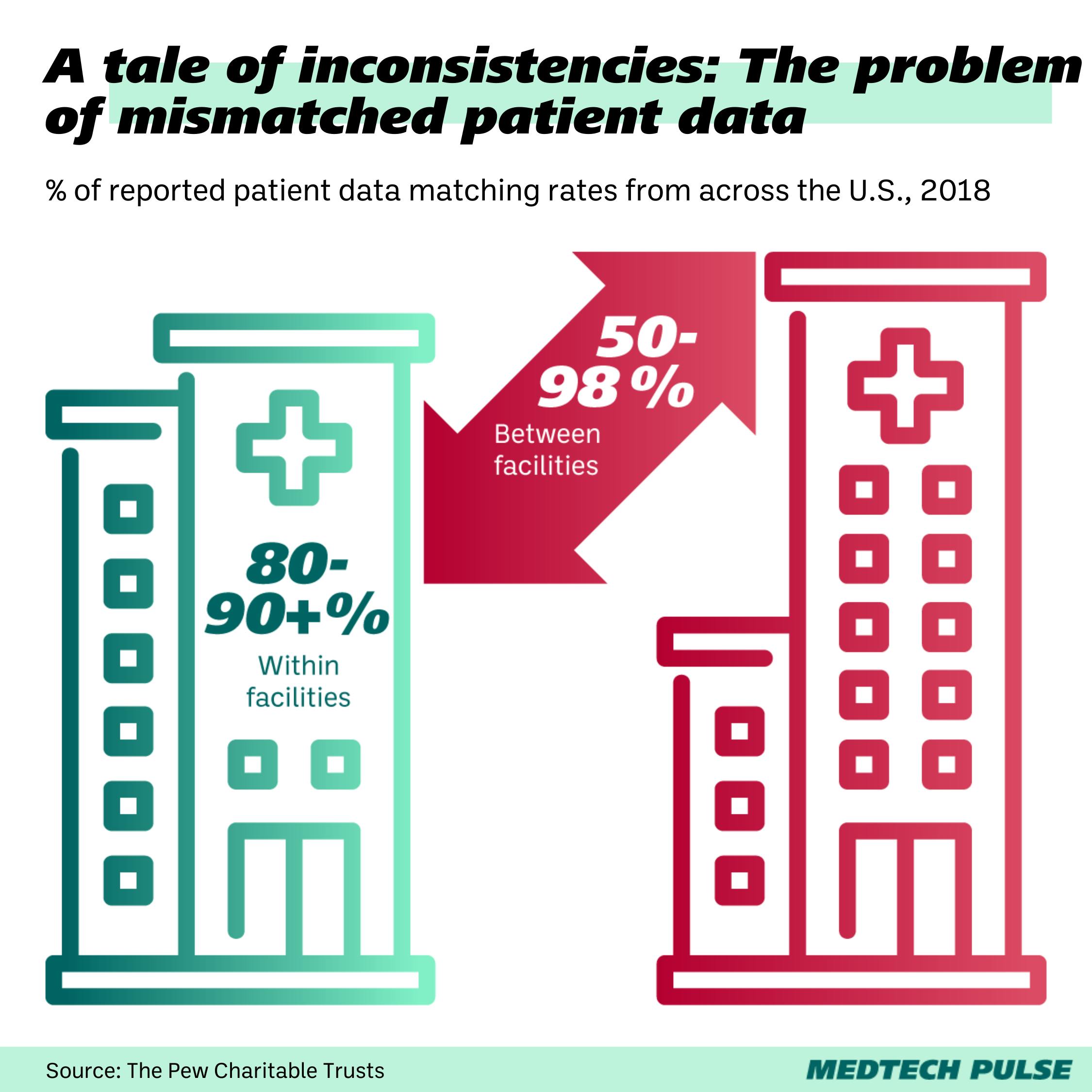
Poor data matching can come down to a few things—like errors in health information exchanges (HIEs) validation procedures on data entry mishaps from health facilities themselves.
Two of the most common culprits? Names and addresses.
If for example, two generations of John Browns have lived at the same address, their Social Security Numbers or patient identification number may be the only ways to tell them apart. Now, let’s say one John spells his name with an ‘H’ and the other doesn’t, but patient intake doesn’t catch the error, his records may be associated with the wrong patient. Another common error: When duplicate records are created for a single patient due to name misspelling or address change.
Now you can see why patient data deduplication by HIEs has become its own area of research.
Using his team’s findings, Wenger is reigniting a charge to fight these errors. One way is by urging legislators to make death data more accessible. At the moment, hospitals mostly rely on state records to confirm patient deaths, and access to these databases (plus cost) varies by state.
But Wenger and his team are also urging health systems to re-examine and update their identity verification and data validation processes.
“If a patient were to call the clinic or a doctor and say a family member died, we don’t necessarily do the best job in documenting that the same way. Physicians don’t know whether that’s stored, the front desk clinic may not be comfortable if they’ve never heard of the patient—they would all document in the note, but not in the official place where it should be,” said UCLA chief medical informatics officer Eric Cheng. “We know we should do it, but we need a little push to do it—and I think this will be helpful for us to demonstrate and prioritize work on this for the rest of the organization.”
At the moment, U.S. hospitals have the option to invest in online obituary or death record mining software from companies like LexisNexis to assist in their death record verification. With the rise in AI-assisted data mining and analysis products, we hope that technology will soon be able to help ameliorate these unacceptable gaps in record-matching.